This series of articles was sparked by the three brief lines on the Connaught Fund website about the history of the Fund and of Connaught Laboratories. The first two articles unpacked the first two lines and set the scene for the third line: “After the 1921 discovery of insulin by U of T researchers Frederick Banting and Charles Best, the lab expanded and began producing insulin as well as other vaccine[s] and antitoxins.” This third article will unpack the last line, focusing on the dynamic story of research and innovation that followed Banting and Best’s discovery of insulin in their small lab, just upstairs from Connaught’s Medical Building headquarters. By 1921, Connaught’s unique evolution within U of T, its physical proximity to that upstairs lab, the personal and pragmatic leadership of its Director, Dr. John FitzGerald, and the pioneering work of his scientific colleagues, would prove vital to producing insulin in a remarkably short time and at an affordable price.

[University of Toronto (UTL), Insulin Digital Library]
[Bliss, Discovery of Insulin, p. 72]

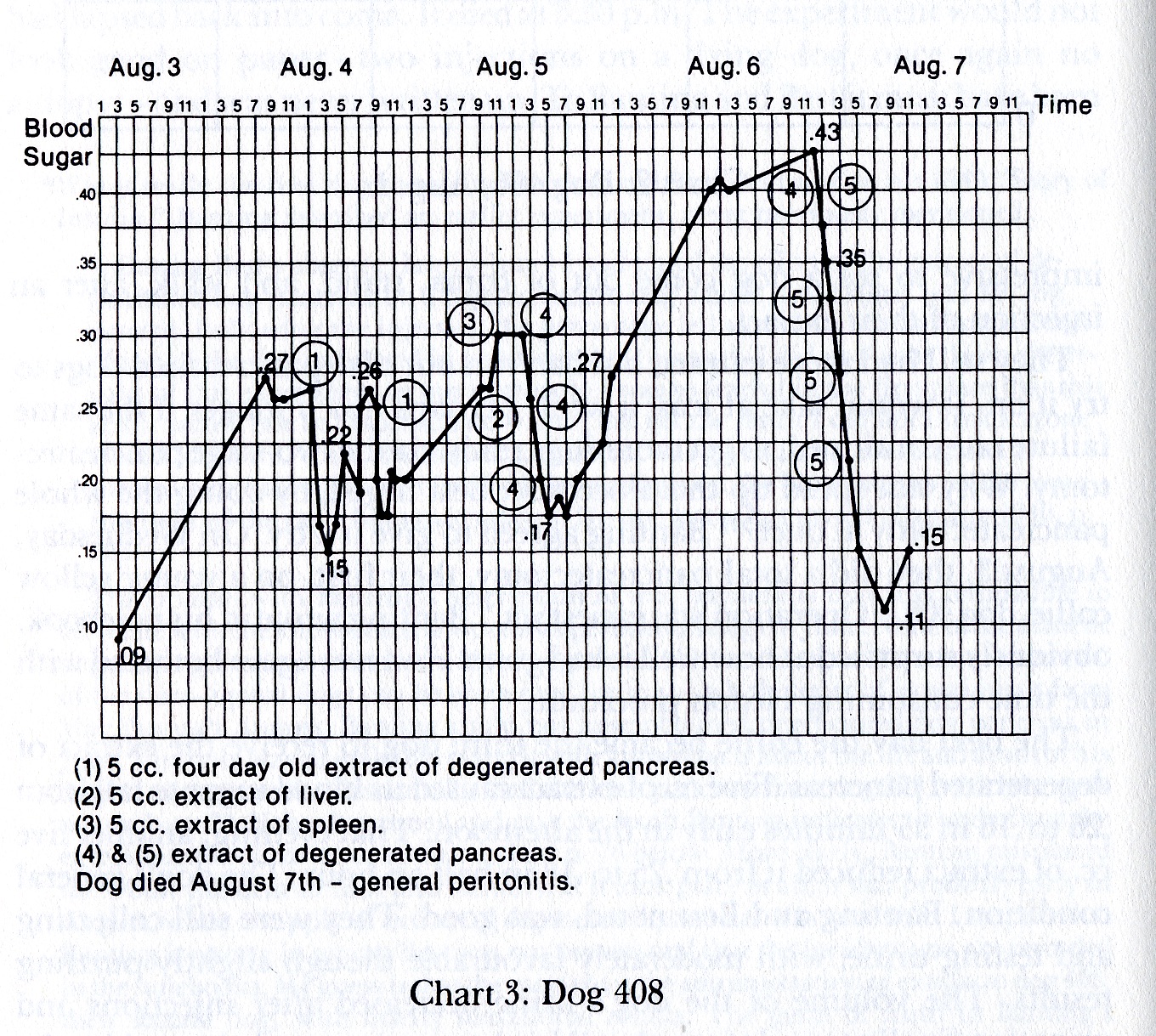
[Sanofi Pasteur Canada Archives]
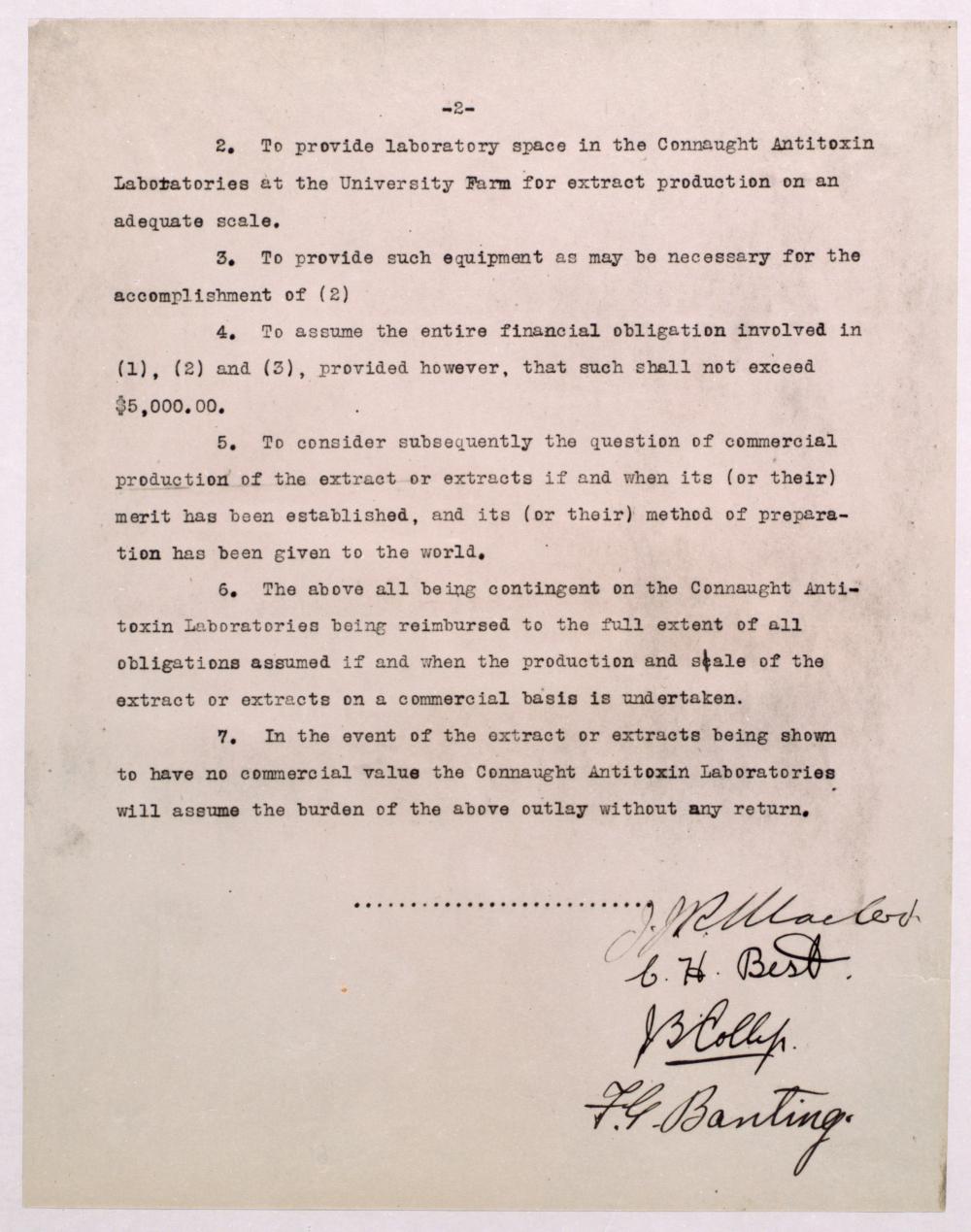
As is well documented by Michael Bliss in The Discovery of Insulin, Banting first visited Dr. John J.R. Macleod at U of T on November 6, 1920, to present his novel idea for how to isolate the hitherto elusive “diabetic principle” from the pancreas. Macleod, Chair of the Department of Physiology and a leading expert on diabetes, was intrigued by Banting’s idea and provided him with a small lab, some dogs he could experiment with, and the assistance of Charles H. Best, a promising medicine and physiology student. Starting in May 1921, Banting and Best worked diligently through an especially hot summer and by early August had prepared a pancreatic extract they called “isletin,” which could reduce blood sugar levels in de-pancreatized diabetic dogs.
[UTL, Insulin Digital Library]
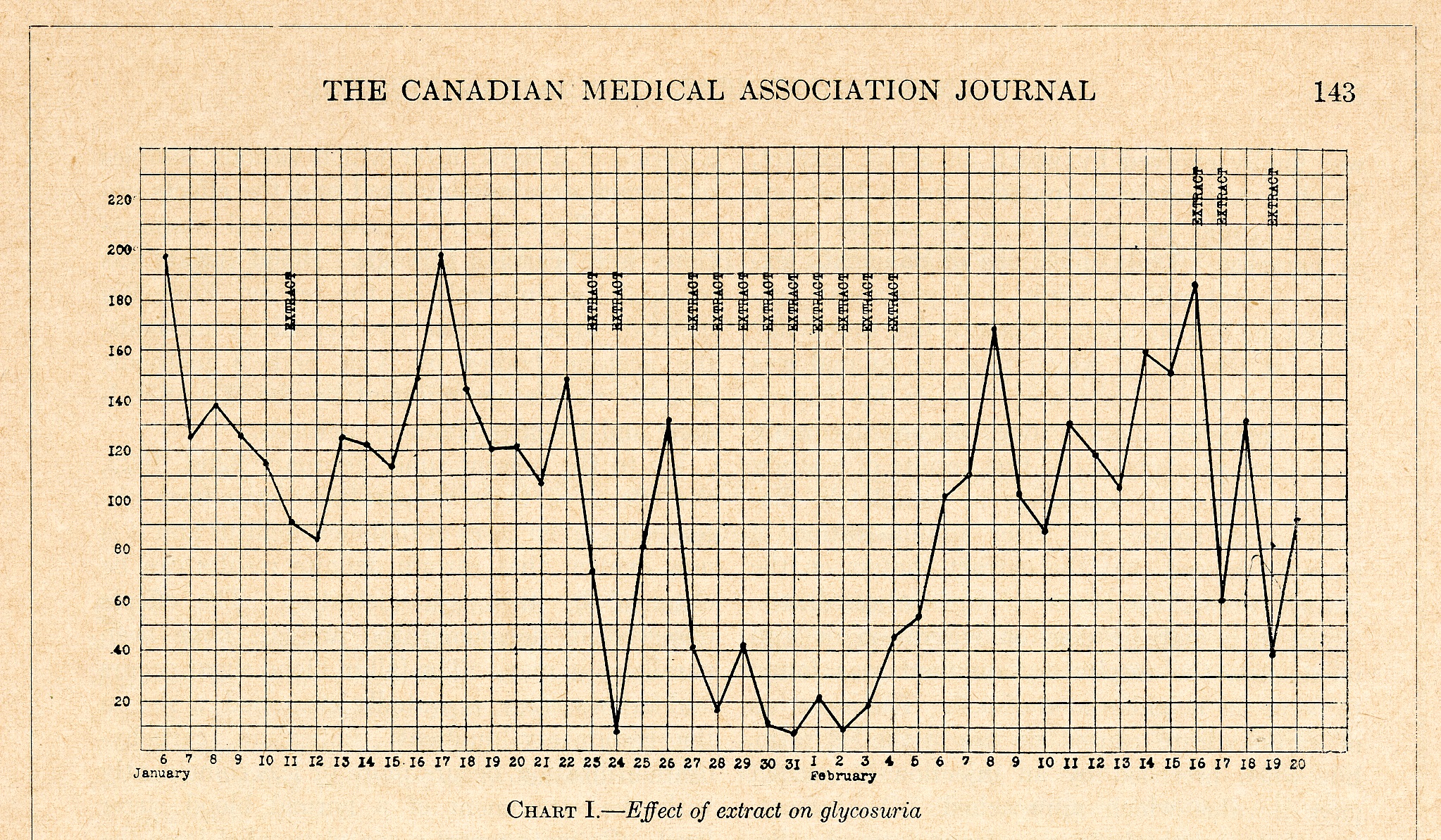
[Canadian Medical Association Journal (March 1922), p. 143]
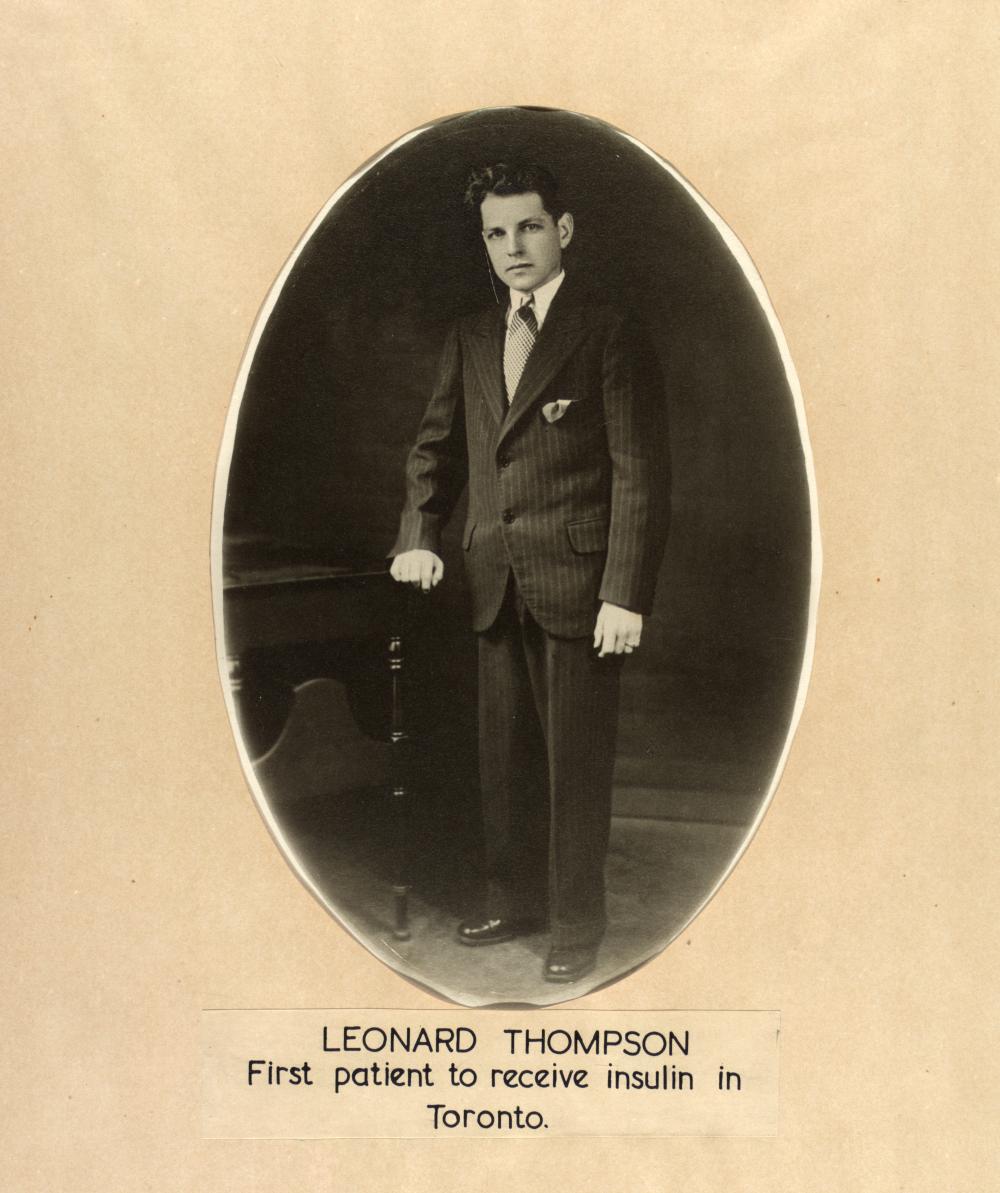
By mid-November, further work had shown that calf pancreas tissue was a more suitable source of the extract. In early December, Dr. James Bertram Collip, a biochemist from the University of Alberta on a sabbatical leave at U of T, joined Banting and Best in preparing a more purified form of the bovine extract that could be tested on diabetic patients. The first successful test was given to 14-year-old Leonard Thompson at Toronto General Hospital on January 11, 1922.
[Sanofi Pasteur Canada Archives]
[UTL, Insulin Digital Library]
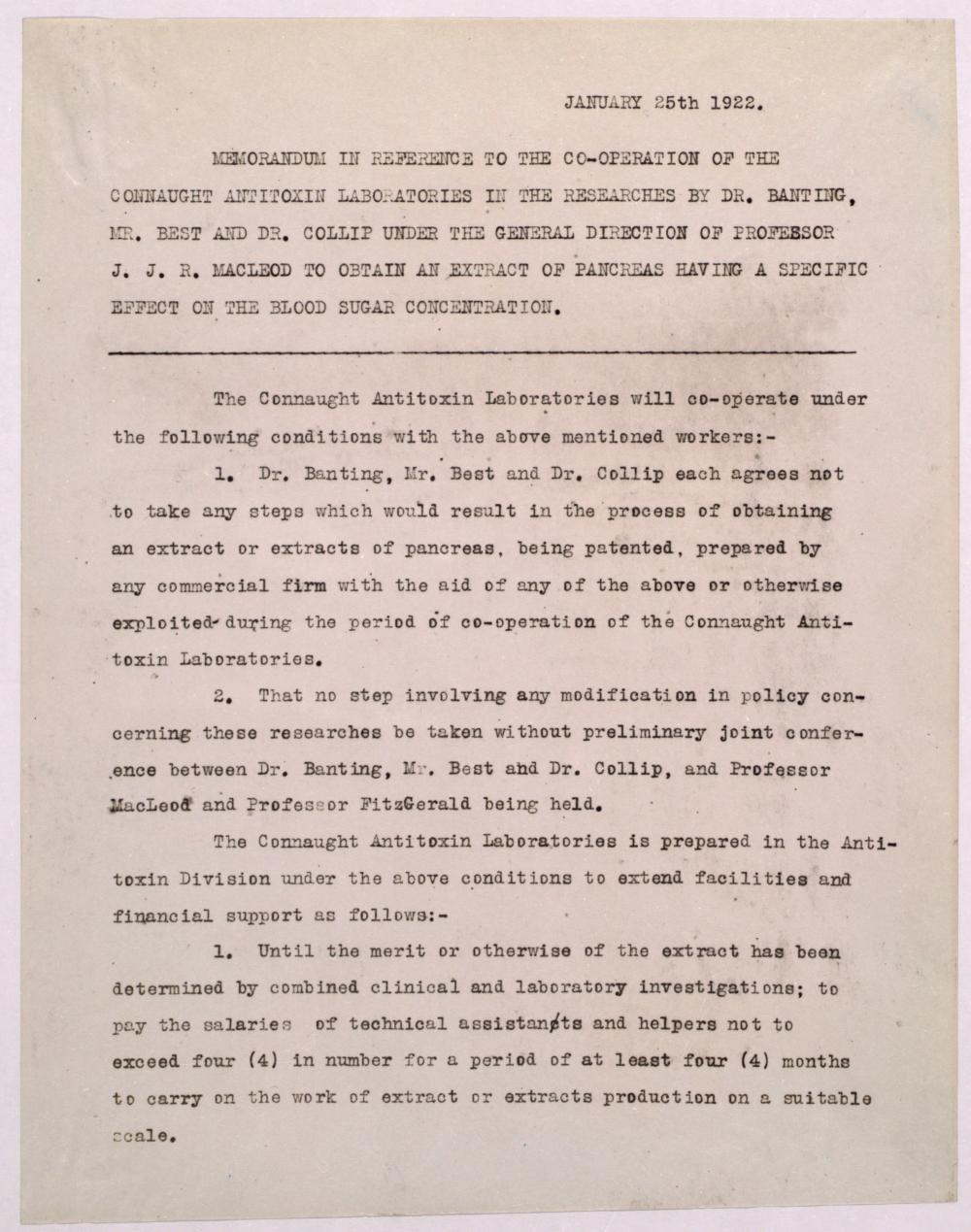
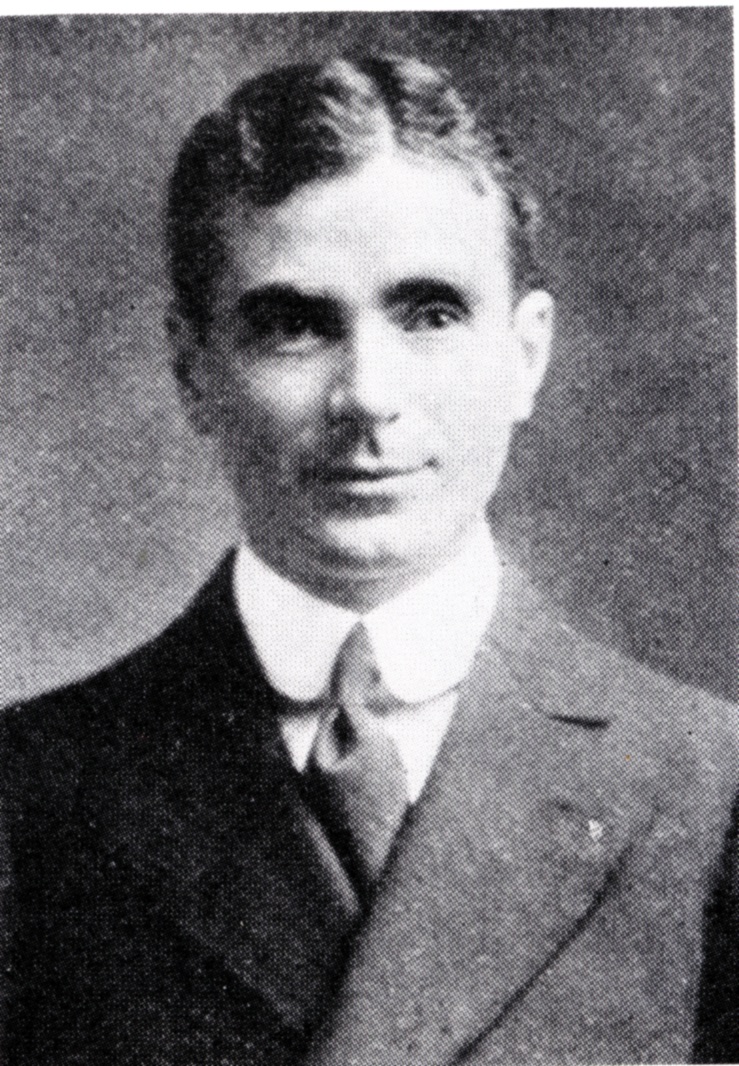
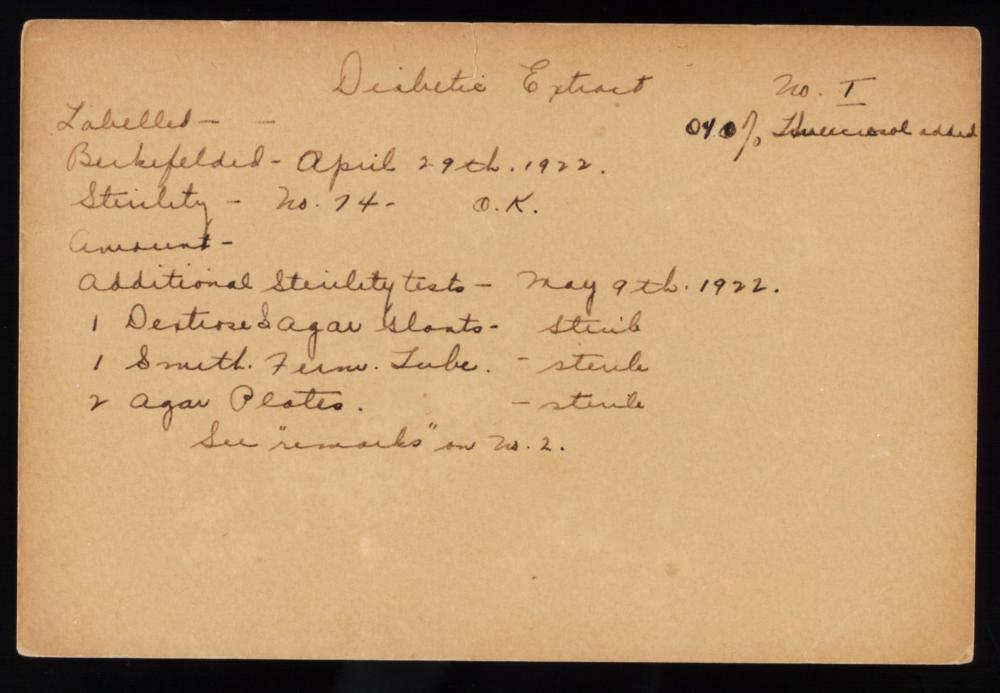
In his Connaught Labs office two floors below Banting and Best’s lab, John FitzGerald would have been well aware of Banting and Best’s initial success with the pancreatic extract. He also very likely attended the November 14th meeting of the Department of Physiology Journal Club, where Banting and Best first presented the results of their research. Indeed, Banting’s experimental work with calf pancreas tissue took place at Connaught’s “Farm” site north of the city, where calves were involved in smallpox vaccine production. Recognizing Banting, Best and Collip’s clear need for space and expertise to prepare and purify the extract on a scale required for clinical testing, FitzGerald offered Connaught’s modest facilities, along with $5,000 from the Labs’ reserves, to help expedite their work. On January 1st, FitzGerald formally appointed Collip and Best to direct Connaught’s production operations in what would later be known as the “Insulin Division.” However, following the first human use of the pancreatic extract, pressure on, and tensions between, the “discoverers” team prompted FitzGerald to personally step in as peacemaker. The tensions stemmed primarily from Collip’s purification work that enabled the first human use and concerns that he could return at any time to Alberta with the method, which he suggested he could patent. To prevent this situation from occurring, FitzGerald led the formalization of a seminal research and development agreement between Connaught and Banting, Best, Collip and Macleod. Dated January 25th, the agreement was based on two key conditions: 1) that the collaborators would sign a contract agreeing not to take out a patent with a commercial pharmaceutical firm during an initial working period with Connaught; and 2) that no changes in the research policy would be allowed unless first discussed among FitzGerald and the four collaborators.
[Bliss, Discovery of Insulin]
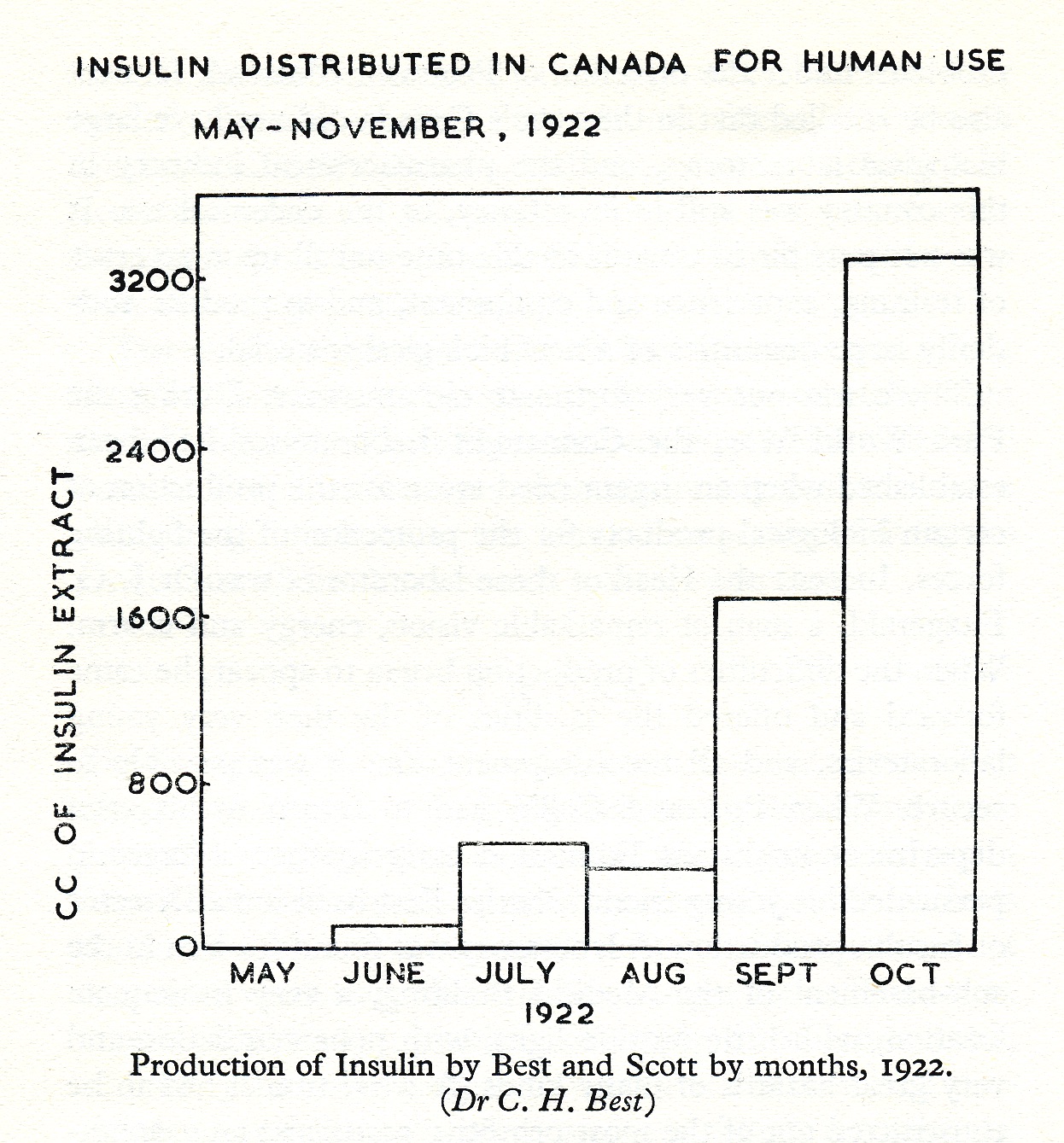
Eli Lilly & Co. of Indianapolis was the first pharmaceutical firm to offer assistance to the U of T to develop the extract, facilitated through the personal efforts of Dr. George H.A. Clowes, who was Lilly’s first Director of Research. Clowes initially offered Lilly’s assistance in December, and then again in March and May, but Macleod was hesitant to work with a commercial drug firm, particularly as Connaught’s facilities were readily at hand. However, as outlined in a joint letter to U of T President from Macleod, FitzGerald, Banting, Best and Collip in May 1922, limits had been reached at the scale to which Connaught could produce the extract, which now was to be called “insulin.” In response to these limits, the joint letter recommended that the university proceed with a collaborative arrangement with Eli Lilly and also accept patent rights in Canada and the United States to safeguard the manufacture and sale of insulin by others, eventually licensing and collecting royalties from other commercial firms that wished to produce insulin. Proceeds from such royalties would be used “to establish a research fund in the University.” The first priority for the funds, however, would be to defray the expenses involved “in testing the efficiency of samples of the manufactured product, because it is highly important for the successful use of ‘insulin’ in diabetic therapy that strict supervision over its production be exercised by us.”[1]
[Sanofi Pasteur Canada Archives]
At Connaught, moving beyond the small laboratory scale was “fraught with many difficulties,”[2] but by the summer of 1922, key advances were made at Connaught that significantly accelerated progress towards increased insulin production. The first of these advances was led by David Scott, whom FitzGerald had personally recruited in the spring of 1922 for insulin development based on his expertise with chemistry and mineralogy. Scott was especially experienced with acetone and pursued the idea of its use in insulin extraction as an alternative to alcohol, since Collip’s original alcohol-based method could not be effectively scaled up. Scott devised a way to replace much of the alcohol with acetone, which was less expensive and easier to work with. This production method gave consistent results during the three months prior to the start of Eli Lilly’s collaboration and was the foundation upon which the company, in close collaboration with Best and several Connaught scientists, further developed larger scale production methods.
[Sanofi Pasteur Canada Archives; UTL, Insulin Digital Library]
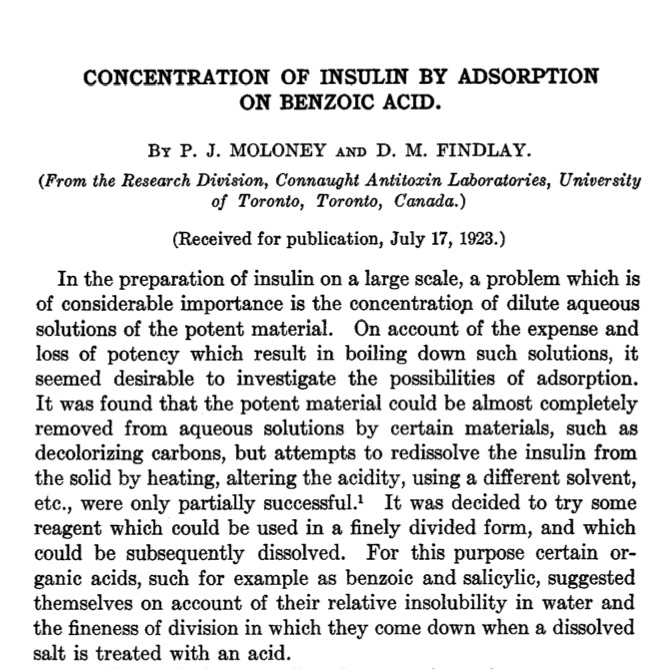
A further critical advance was made by Dr. Peter J. Moloney, Connaught’s first research chemist, originally recruited in 1919 by FitzGerald to focus on improving the purification of diphtheria antitoxin. Before pH meters were available, Moloney developed a quick-acting hydrogen electrode, known as the “Moloney Electrode,” designed to more accurately and rapidly determine the acidity of bacterial culture broths used in antitoxin and vaccine production; it also proved useful for measuring the pH during insulin production. The importance of preparing more purified insulin quickly grew apparent after its initial human clinical use and it was on this particular challenge that Moloney focused his attention. Moloney’s insulin work was based on research involving the purification of proteins, which he had been involved in at the federal Department of Agriculture in Ottawa, prior to joining Connaught. The expense and loss of potency inherent in the boiling down of such solutions suggested to Moloney that a better approach would be through the adsorption of proteins from aqueous solutions using certain materials, one of which was sodium benzoate, which was relatively insoluable in water but could be subsequently dissolved in an acid. Thus, as Moloney described in his paper, “Concentration of Insulin by Adsorption on Benzoic Acid,” the potent protein material in an aqueous solution of pancreatic extract (insulin) could be removed by adding sodium benzoate, which would adsorb the protein. And when an acid was added, the sodium benzoate would dissolve and the protein (insulin) would precipitate out of the solution.[3]

[Defries, First Forty Years, p. 77]
[Moloney and Finlay, Journal of Biological Chemistry 61 (1923), p. 359]
The benzoic acid method marked a distinct advance in large scale insulin production: by using this process, minimal amounts of alcohol and/or acetone needed for the fractional precipitation of the proteins and the final precipitation of insulin were required. The final insulin product was much freer of protein material than had been previously possible, resulting in far fewer toxic and indurating effects when administered clinically. Although this method involved tedious filtration steps that limited its ultimate utility, some 250,000 units of insulin using the benzoic acid method were produced at Connaught and used clinically in Toronto during the fall of 1922, with “very satisfactory results,” according to Best and Scott.[4]
[Wrenshall, Hetenyi, Feasby, The Story of Insulin, p. 78]
By early November, Connaught was producing about 1 litre of insulin per week. Connaught’s more consistent and larger insulin production capacity had been significantly supported by new equipment made possible by a gift of $10,000 from Mr. Bacon of New York City. He was a patient of a prominent diabetes specialist, Dr. Greylin, who facilitated the gift through Banting.
[Sanofi Pasteur Canada Archives; UTL, Insulin Digital Library]
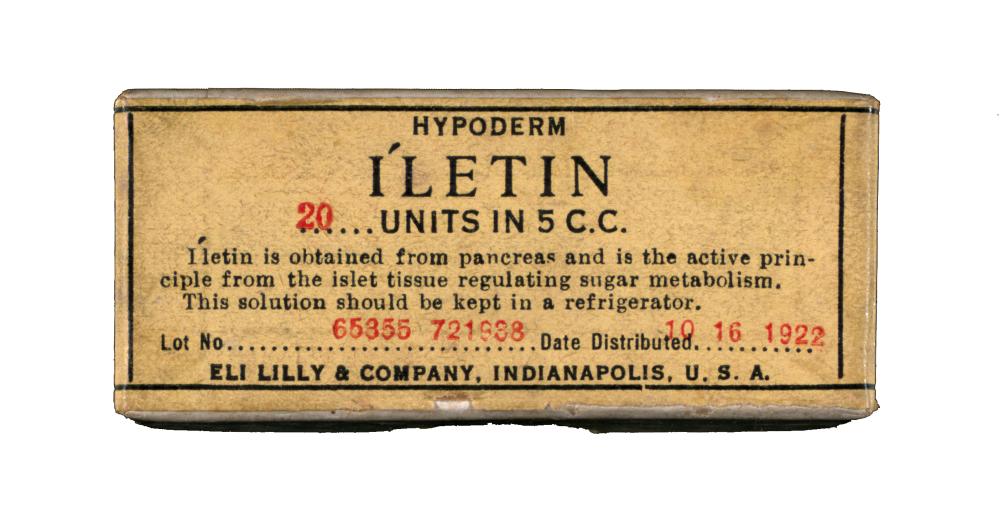
In the meantime, at Eli Lilly, insulin production progress had been frustratingly slow (Lilly used “Iletin” as its brand name), the cause of an especially serious stability problem traced to varying pH levels between batches. After closely tracking pH levels, George Walden, the research chemist at Lilly, observed that insulin was being precipitated out of the insulin solution at the “wrong” pH—precipitate that was far purer and potent than hitherto seen. The key was to determine the optimum “isoelectric point,” or pH at which a particular molecule (i.e. insulin) carried no net electrical charge and would precipitate out of the pancreatic extract solution. Subsequently, Walden deliberately adjusted the pH of the pancreatic extract solution to the isoelectric point for insulin to cause the maximum precipitation. However, Walden was not the only scientist to observe the “isoelectric point” for insulin. At about the same time, Dr. Phillip Shaffer at Washington University in St. Louis stumbled upon the “isoelectric point” for insulin. Lilly had hoped to win an insulin production patent for itself based on the “isoelectric point,” but after learning about Shaffer’s very similar observation through the U of T Insulin Committee, Lilly could not reasonably proceed. Thus, through the efforts of Connaught’s Assistant Director, Robert Defries, and the Insulin Committee, an innovative patent pooling policy was established. As was outlined by the Committee in April 1923, “it shall be required of all licenses that any patents taken out by them shall be assigned to the University of Toronto who may then authorize other licensees to use the methods patented, in other words the policy of pooling the patents was decided upon.”[5]

[Sanofi Pasteur Canada Archives; UTL Insulin Digital Library]
During the spring of 1923, Defries was managing Connaught’s operations while FitzGerald was on a sabbatical at the University of California in Berkeley. Defries juggled two insulin issues: 1) how to distribute in Canada the surplus of insulin that had built up, and 2) how to expand the insulin production facility at Connaught. The first issue was dependent upon training physicians in other provinces on the proper clinical use of insulin, based on the experience in Ontario. An initial strategy was to invite selected physicians from around the country with a special interest in diabetes to Toronto to receive specialized instruction on the use of insulin, including from Banting. To solve the second challenge, Defries required a suitable space and sufficient funds for the needed equipment.
[The Globe, August 1, 1923, p. 11]
The most immediate issue was finding the space, and in early April a potential site was found on campus not far from the Medical Building. The U of T’s YMCA facility was planned to be torn down but when Defries heard about it, he was given approval to take over the vacant building. Defries then personally approached Ontario Premier, E.C. Dury, who committed $25,000 from the provincial government to transform the former YMCA building into an insulin factory. Connaught’s reserves and private donations provided the balance of funds to cover the total of $43,000 required to complete the job. As Defries told the press in mid-May, Connaught would now be able to produce enough insulin for all of Canada in the new facility and at a steadily declining price.

[Sanofi Pasteur Canada Archives]
On August 1st, an article in The Globe newspaper noted that work on the building had been partially completed and that Charles Best, head of the Insulin Division, had already moved into his office. The article also emphasized that insulin would be produced commercially nowhere else in Canada, and that Connaught’s facility would “provide the curative fluid for all countries which do not manufacture their own supply.”[6] By November, Connaught was producing 250,000 units of insulin weekly; the average diabetic needed 15–20 units every day. Best worked closely with David Scott, managing insulin production with a staff of 26 working 24/7 to keep up with demand in Canada and beyond; insulin was now being exported from Toronto to Ireland, South Africa, New Zealand, and Australia, as well as to several other countries without their own production facilities. The price the Labs charged for insulin—as was true for all of its vaccines and antitoxins—was governed entirely by the costs of materials and production, since Connaught was “not engaged in commercial business.” After returning from his sabbatical, FitzGerald focused on the Labs’ broader long-term needs, including a larger and better equipped insulin production facility, as well as a facility to accommodate an expanded research and teaching capacity in the Department of Hygiene. A potential solution arose through the Rockefeller Foundation, based in New York City, which was already impressed with the innovative public health services that had developed in Toronto between U of T, especially through Connaught, and the Department of Public Health, the Provincial Board of Health, and local hospitals. The Rockefeller Foundation had previously provided funding to U of T’s Faculty of Medicine in 1920 and offered $10,000 to support Banting’s clinical studies of insulin. However, it was looking for an institution to further showcase its growing philanthropic support for public health education and research. Rockefeller funds had established schools of public health at Johns Hopkins University in 1918 and at Harvard in 1921, and the University of Toronto seemed the obvious choice for creating a third such school in North America. When Rockefeller officials met with FitzGerald in 1923, Connaught’s Director was not shy about highlighting the Labs’ needs. How that meeting led to the creation of U of T’s School of Hygiene, and how its establishment further shaped the insulin story as well as Connaught’s pioneering vaccine work during the balance of the 1920s, especially its prevention of diphtheria, will be the focus of the 4th article in this series.

[Sanofi Pasteur Canada Archives]
[Toronto Star, Nov. 29, 1923]
Useful Resources:
Bator, Paul with Andrew J. Rhodes: Within Reach of Everyone: A History of the University of Toronto School of Hygiene and the Connaught Laboratories, Volume 1, 1927-1955 (Ottawa: Canadian Public Health Association, 1990) Bliss, Michael: The Discovery of Insulin (Toronto: McClelland & Stewart, 1982) Clowes, Alexander W.: The Doc and the Duchess: The Life and Legacy of George H.A. Clowes (Indianapolis: Indiana University Press, 2016) Defries, Robert D.: The First Forty Years, 1914-1955: Connaught Medical Research Laboratories, University of Toronto (University of Toronto Press, 1968) FitzGerald, James: What Disturbs Our Blood: A Son’s Quest to Redeem the Past (Toronto: Random House, 2010); details at: http://www.jamesfitzgerald.info Moloney, Mary V.: Behind Insulin: The Life and Legacy of Peter Moloney; A Man’s Catholic Faith and Bold Science (Toronto: Lulu, 2016); book available via http://www.drpetermoloney.com/ Rutty, Christopher J: “’Couldn’t Live Without It’: Diabetes, the Costs of Innovation and the Price of Insulin in Canada, 1922-1984,” Canadian Bulletin of Medical History 25 (2008): 407-31; article available at: https://www.utpjournals.press/doi/abs/10.3138/cbmh.25.2.407 Rutty, Christopher J. and Sullivan, Susan: This is Public Health: A Canadian History (Canadian Public Health Association, 2010), online eBook: https://www.cpha.ca/history-e-book Sanofi Pasteur Canada, “The Legacy Project”: http://thelegacyproject.ca University of Toronto Library: “The Discovery and Early Development of Insulin” Digital Library; https://insulin.library.utoronto.ca/ “Within Reach of Everyone: The Birth, Maturity & Renewal of Public Health at the University of Toronto,” Dalla Lana School of Public Health website feature: http://www.dlsph.utoronto.ca/history/ Wrenshall, G.A., Hetanyim G, and Feasby, W.R.: The Story of Insulin: Forty Years of Success Against Diabetes (London: The Bodley Head, 1962)
Endnotes:
[1] J.J.R. Macleod, J.G. FitzGerald, F.G. Banting, C.H. Best (and J.B. Collip?) to Robert Falconer, May 25, 1922, University of Toronto Archives (UTA), Accession A1982-0001, Box 13, file 11. [2] Ibid. [3] P.J. Moloney and D.M. Findlay, “Concentration of Insulin by Adsorption on Benzoic Acid,” Journal of Biological Chemistry 57(2) (Sept. 1923): 359-61 [4] C.H. Best and D.A. Scott, “The Preparation of Insulin,” Journal of Biological Chemistry 57(3) (Oct. 1923), p. 715. [5] University of Toronto Insulin Committee Meeting, April 10, 1923, UTA, Accession A1982-0001, Box 44, file 1. [6] “New Laboratory,” The Globe, Aug. 1, 1923, p. 11.
